Joint stability is further reinforced by the capsule (strong surrounding ligaments) and the labrum – a specialized ring of fibrocartilage that originates from the rim of the socket and forms a suction seal against the femoral head. Dysplasia is a congenital disorder in which the hip socket does not cover the ball part of the joint well, leading to poor function of the hip joint. This can be from suboptimal position of the socket, low socket volume, or both which then gives rise to hip instability, or excessive translational motion and increased shear forces within the joint. Typical anatomic abnormalities in acetabular dysplasia include shallow socket, enlarged labrum, ligamentous laxity or loose ligaments, and/or excessive hip internal rotation or femoral antetorsion.

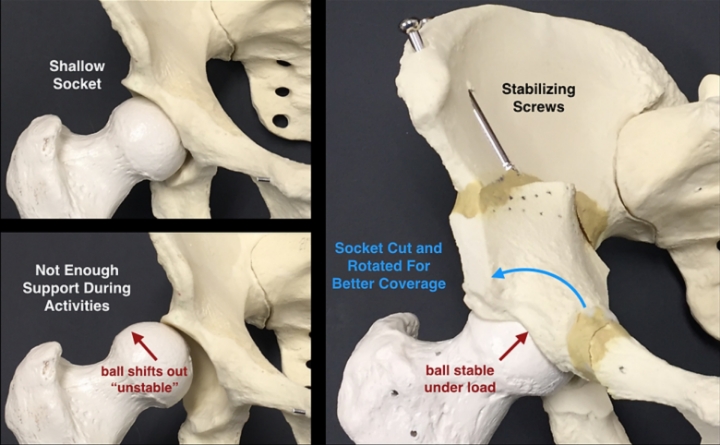
Acetabular dysplasia, or dysplasia, is a congenital and/or developmental disorder in which the hip socket is too shallow or/and steeply oriented to adequately house the ball. Dysplasia is most commonly seen in females who have generalized ligamentous laxity allowing them to hyperextend their elbows, wrists, and knees. The shallow socket gives rise to hip instability, or excessive translational motion and increased shear forces within the joint. Typical anatomic abnormalities in acetabular dysplasia include:
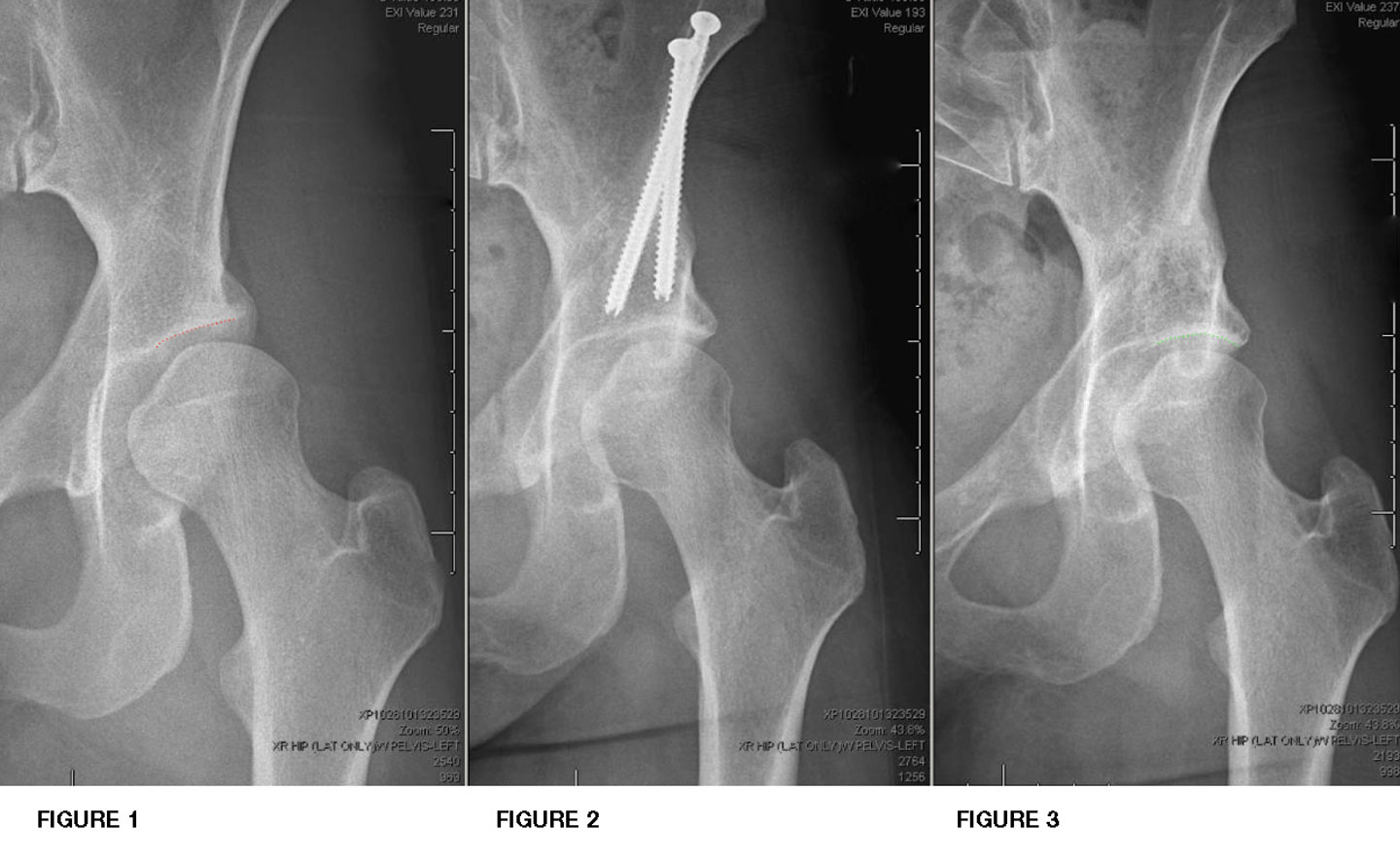
The natural history of acetabular dysplasia is well documented and varies with the severity of dysplasia. Dysplasia is rated as either borderline or frank, with frank being the more severe variant. Patients with frank dysplasia typically experience progressively worsening pain until the hip deteriorates to end-stage arthritis. Some studies have reported that the time to progress to severe arthritis may be as little as 5 years from the onset of symptoms. This makes frank dysplasia a semi-urgent condition for which time is of the essence. Delaying treatment may result in the accumulation of significant cartilage damage, which may then preclude a corrective osteotomy, making joint replacement the only viable option.
The natural history of borderline dysplasia is less clearly defined, and there is ongoing research in this area of hip preservation with the goal of establishing clear treatment algorithms. Dr. Mei-Dan approaches the treatment of borderline dysplasia on a case-by-case basis, incorporating the latest scientific evidence into his decision-making algorithm. Some borderline dysplastic patients may be adequately treated with minimally invasive arthroscopy alone, while some require a corrective realignment osteotomy.
Dr. Mei-Dan will discuss the important factors that enter into this complex algorithm to achieve the best possible results.
The first line of treatment is conservative management, consisting of activity modification to avoid positions of instability, physical therapy to strengthen the surrounding musculature, and various injections to reduce inflammation and provide temporary relief (we strongly discourage steroid injections as they have the propensity to damage joint’s cartilage). When these measures fail to provide adequate relief of symptoms, the next step is to surgically correct the underlying structural abnormality.
Surgery for dysplasia is tailored to each patient’s unique hip morphology to comprehensively address all sources of instability. A hip arthroscopy is first carried out to address any labral or cartilage tears, joint inflammation, and impingement anatomy. Following arthroscopy, patients may require a periacetabular osteotomy (PAO) and/or a derotational femoral osteotomy (DFO), depending on the unique pathomorphology. The second surgery is typically performed ~1 week following hip arthroscopy to allow for early rehabilitation and to prevent scar tissue formation.
We stage the hip scope and the PAO a minimum of 5-7 days apart. The main reasons for this methodology lay in the clinical and technical implications laid out below:
The number one reason cited by published studies and surgeons worldwide for continued pain after hip scope / need for revision hip scope surgery is scar tissue formation, or adhesions in the joint. The main driver for adhesions forming between the capsule and labrum is bleeding associated with labral repair and cam resection procedures. The best way to prevent adhesions is mobilizing the joint. Patients must spend up to 30 minutes daily on a stationary bike after a hip scope (starting with 5-10 minutes a few times daily) to push the bleeding out of the joint, dry the joint out and reduce the chances for scar tissue formation, both inside and outside (around) the joint. Contrastingly, after a PAO procedure, patients cannot ride a stationary bike for several weeks.
Dr. Mei-Dan performs both the hip scope and the PAO (or/and DFO) surgeries, which is considered unique in the field. Most hip procedures require providers who trained via completely different pathways and possess very different skill sets to enable them to execute these unique procedures, encouraging surgeons to focus on one particular procedure. Dr. Mei-Dan has devoted many years and ample resources to master two unique, complex procedures, affording patients the luxury of a highly-skilled, knowledgeable, multi-specialized provider. For the patient, this translates to innumerable synergies. Dr. Mei-Dan is able to leverage knowledge gained from the hip scope (i.e. knowing exactly how the joint looked from the inside) in future procedures such as a PAO, ensuring nothing falls through the cracks and there are no misunderstandings or disagreements between different providers regarding the optimal way to complete the next steps in the care plan.
In order to prepare for each patient’s surgery and formulate a tailored per-patient strategy, Dr. Mei-Dan reviews all that was evidenced and performed during the scope, ties that to the exhaustive history of every patient, their imaging sets and exam findings, and then formulates an optimal plan for the PAO. This methodical, painstaking and time-intensive approach is instrumental to surgical success and outcome. These procedures are undertaken carefully, and are intentionally not rushed.
A PAO is a major undertaking for both the patient and the surgeon, with one main goal in mind – a long-term, pain-free hip. The proper measures are taken to ensure clinical success, and procedures are not rushed in favor of maintaining an arbitrary timeline. The future, positive outcome – grounded in both the careful refinement of the hip socket alignment and the delicate balance of the newly adjusted hip range of motion required for different sports and life activities – is the priority for our patients, and we take the necessary time to achieve this outcome.
In addition to clinical factors, there are also social, financial and psychological factors that lend themselves to staged procedures:
Lastly, many patients understandably tend to be anxious before a major surgery such as a PAO. This may be due to the required time commitment, magnitude of the procedure and misinformation online (patients seeking treatment from inexperienced or low-volume surgeons are more likely to experience negative outcomes, and distribute them online).
A hip scope is a relatively easy procedure to recover from. Patients generally report experiencing only mild pain for a few days, which helps boost confidence and reduce potential anxiety about future procedures.