The hip is a synovial joint that is lined with smooth articular (surface) cartilage. The joint is further lubricated with synovial fluid (joint fluid) creating a low friction environment for the femur (ball) to rotate and glide within the acetabulum (socket). Depending on the type of activity, forces transmitted across the hip joint can be several times the entire body weight of a person, placing significant load on the cartilage. Healthy cartilage is able to withstand these loads through numerous adaptations:
The surface cartilage is made of cells (1%) surrounded by a water-based matrix (99%), which contains collagen along with various other proteins that attract water. The water moves out of the matrix and into the synovial fluid when a load is placed across the joint, and returns when the load is released (like a sponge). This water action dissipates much of the load by conferring a spring-like quality to the cartilage. As the cartilage becomes damaged and calcified (with progressive osteoarthritis) this function is compromised.
There are two types of cartilage damage in the hip: focal, which is common in FAI and hip dysplasia, and generalized, which corresponds more with hip OA.
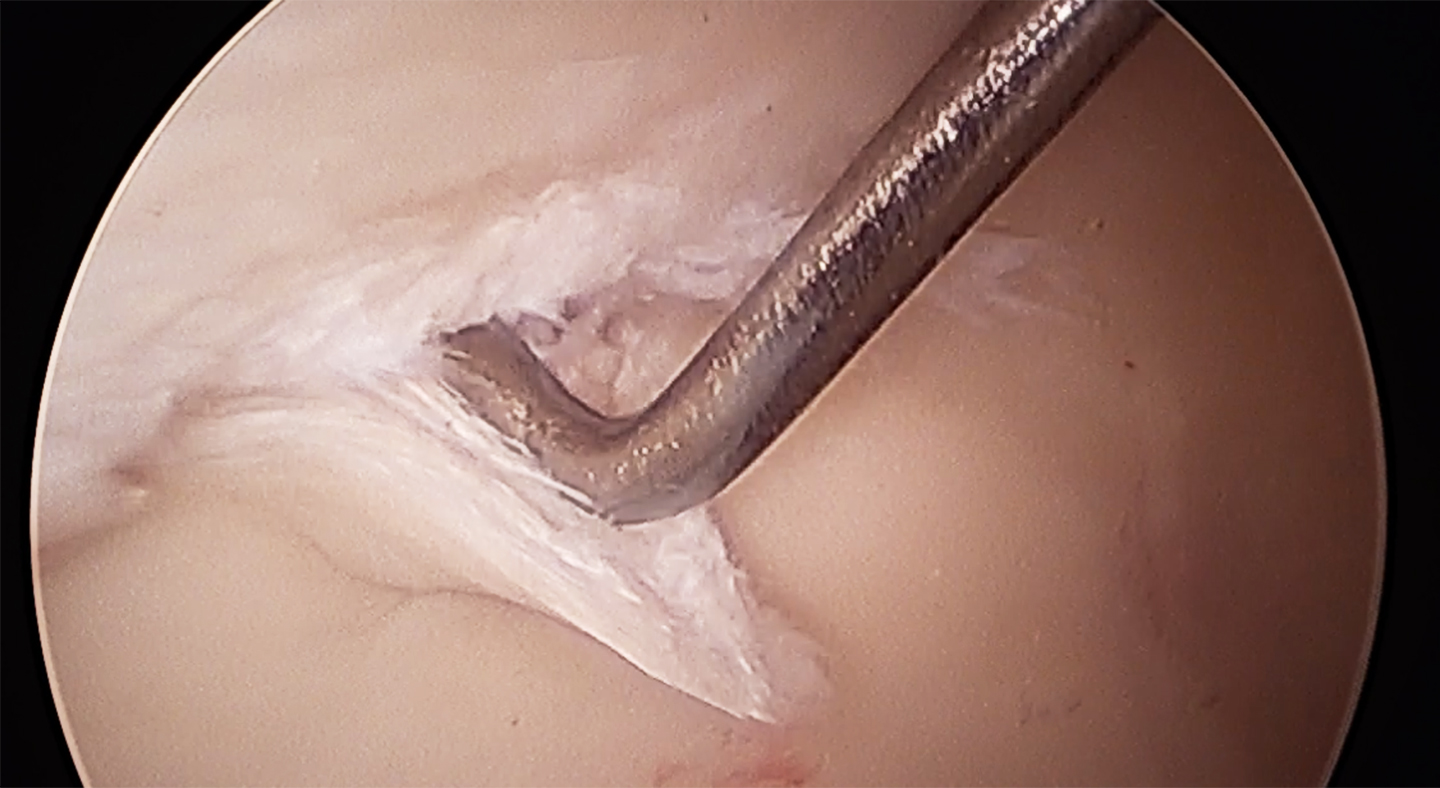
Focal cartilage damage typically occurs in the setting of an injury (hip dislocation) or over time with long-standing hip impingement (FAI) or hip instability (dysplasia). The area of damage (lesion) is typically a well-circumscribed defect with healthy neighboring cartilage. The severity of the defect ranges from mild softening (Grade I) to exposed underlying bone that is missing its overlying cartilage (Grade IV). Lesions that are Grades I – III are typically treated with shaving and debridement, while Grade IV lesions are addressed with various cartilage restoration and regeneration techniques.
Generalized cartilage damage affects the majority of the surface cartilage and can come about over time with untreated focal lesions or with osteoarthritis. The goal is to address cartilage damage before it becomes generalized and treatment options are limited. Unfortunately, minimally invasive hip arthroscopy is not a good option for patients with significant (Grades III & IV) generalized cartilage damage, as it is impossible at this point in time to regenerate a large area of cartilage loss. Platelet-rich-plasma (PRP) injections may be of benefit for patients who want to maintain an active lifestyle and are not ready for the risks and limitations of a hip replacement. Otherwise, the only viable long-term treatment option is joint replacement surgery.
Surface cartilage is best visualized with magnetic resonance imaging (MRI) utilizing specialized sequences (or ways of running the scan) to isolate and enhance the cartilage sequences. A more comprehensive analysis of surface cartilage composition can be obtained with a delayed gadolinium enhanced-MRI of cartilage (dGEMRIC) scan, using contrast material injected through an IV, however this technique’s values don’t always correlate with surgical outcomes thus not commonly used.
When surface cartilage damage is restricted to a focal, well-circumscribed area with healthy neighboring cartilage there are several methods by which new cartilage growth can be achieved to “fill-in” the defect:
Microfracture procedures work better in the hip socket compared to the knee, because the hip is a much congruent ball and socket joint which tends to distribute the stresses better and contain the lesion optimally. This enables the new forming cartilage to develop in a “protected” environment as long as the patient maintains non weight bearing status for 6 weeks, avoiding shearing stress to this new forming tissue.
However, if microfracture failed to “take”, meaning the cartilage did not grow well into the defect, we may use advanced cartilage procedures where we use autologous or allogeneic cartilage tissue which is implanted into the defect. There are currently different options available to us, and we will tailor these per lesion size, location and patient’s inherent characteristics. These procedures are still done Arthroscopically.
Dr. Mei-Dan developed several cutting edge techniques and devices to be able to graft cystic cavities in the hip socket and femoral head. These cysts develop usually in association with hip dysplasia and more rarely with Hip FAI. Previously surgeons did not deal with these cavities due to lack of proper tools and techniques. Our published mid term results of grafted cysts followed by anatomical correction of the pathology (i.e PAO for instability, or cam resection form FAI) shows minimal difference compared to surgeries where we did not encounter cysts. This is very promising as traditionally surgeons consider these cysts as contra-indication for hip preservation procedures, even in young patients.
The integrity or health of the surface cartilage is by far the most important consideration when choosing between different treatment options for any hip disorder. Patients can take several steps to ensure that their hips remain healthy for years to come: